
OSTEOARTHRITIS
FIVE COMMON MYTHS ABOUT WHAT IT IS AND HOW TO MANAGE IT
“Is It Arthritis?”
This is one of the most common questions that we get asked as physio’s when we assess a new client. Often people are really worried (understandably!) about the dreaded “arthritis” word. This is because the common belief is that “Well, it’s arthritis so there’s nothing much I can do, it’ll probably get worse, and I should stop playing sport or doing exercise because it’ll just wear the joint out quicker”. Thankfully, while this belief is really common, it’s also incorrect.
Firstly it’s important to remember that there are several different types of arthritis – osteoarthritis (OA), Rheumatoid arthritis, Psoriatic arthritis etc… In this issue we’ll only be talking about osteoarthritis – OA. This is because it’s the most common type of arthritis, and also because it’s part of our normal ageing process. A recent study (Culvenor et al 2019) showed that 19-43% of asymptomatic adults aged over 40 had MRI findings of OA. Basically, we almost all get OA to some degree even though many people will not have any pain.
Think of OA as a normal process of two joint surfaces sliding against each other over the years – you’d expect a bit of wear and tear to take place. This is different to other types of arthritis, where there is usually some form of active disease or pathology going on. So the process of diagnosing and managing other types of arthritis is different to OA.
If Everyone Gets Osteoarthritis Then Why Doesn’t Everyone Have Pain?
One of the main things to remember about OA is that two different people with similar amounts of OA shown on x-ray can report very different levels of pain and functional restriction. This means that someone with a lot of OA shown on x-ray can actually have minimal pain, whilst someone else with relatively mild OA (as shown on x-ray) can report high pain levels. This is because the actual amount of joint wear and tear shown on x-ray is only one factor in your body and brain’s response to the OA process, as we discuss below.
To help you understand this complex relationship and how it helps us effectively manage OA, lets review the top five common myths about this common type of arthritis.
MYTH 1: I Need An X-ray Or MRI To Diagnose If I Have Osteoarthritis
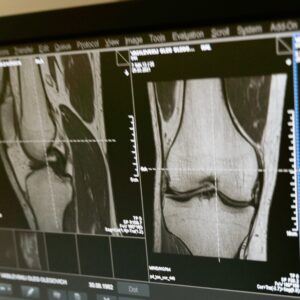 The Royal Australian College Of General Practitioners guidelines (RACGP, 2018) support the use of clinical assessment for diagnosing OA without the need for imaging. Following this recommendation helps avoid unnecessary x-rays or MRI’s which reduces your exposure to unnecessary radiation, reduces waiting times for other more important scans, and saves money for both you and Medicare (and therefore our tax system).
The Royal Australian College Of General Practitioners guidelines (RACGP, 2018) support the use of clinical assessment for diagnosing OA without the need for imaging. Following this recommendation helps avoid unnecessary x-rays or MRI’s which reduces your exposure to unnecessary radiation, reduces waiting times for other more important scans, and saves money for both you and Medicare (and therefore our tax system).
The RACGP (2018) guidelines only recommend imaging for people whose presentation does not fit the usual pattern for OA. This may include if they have a history of trauma or significant injury, a rapid worsening of symptoms, they have a hot swollen joint, or other potential red flags (unexplained symptoms that may indicate a serious underlying pathology).
As mentioned above, we need to remember the really variable relationship between the amount of OA shown on imaging and the amount of pain felt by the person. This is important because our beliefs about our condition have a big impact on how we perceive our symptoms. So, if a client with mild/moderate symptoms is referred for an x-ray which shows some advanced OA they may suddenly feel that their problem is much worse than they thought, and they can actually start feeling more pain purely because their imaging showed more significant OA than they thought.
I know this sounds strange – that someone’s pain levels can change purely based on how bad they think the problem is – but it is a very well-researched and proven part of our complex pain response. It forms part of what is called the Biopsychosocial Model of Health.
Another reason why imaging is not used early to diagnose OA is that it usually doesn’t change our management plan. If the results of a scan are not going to change or improve your treatment or recovery, then there is not much point in having it. Instead, physio’s base our management plans on a comprehensive client history and physical examination. We focus on the most important things for you that your pain is stopping you doing, then assess how physical factors such as your mobility, strength and movement control are contributing to these limitations. From there we put a management plan in place to correct these things and ensure that this allows you to get back to doing the things you love.
MYTH 2: The More Wear And Tear I Have In My Joint, The More Pain I Will Have
 As mentioned above, the amount of pain you feel is not directly proportional to the amount of OA (i.e. joint wear and tear) shown on imaging. OA symptoms can actually occur before any structural changes appear on imaging.
As mentioned above, the amount of pain you feel is not directly proportional to the amount of OA (i.e. joint wear and tear) shown on imaging. OA symptoms can actually occur before any structural changes appear on imaging.
This is because when we experience pain it is not just a message to our brain from a damaged structure in our body, like a joint or muscle. Pain is a complex and personal experience that is modified in our brain by our past experiences, mental state, emotions, beliefs, mood and social situation. This means that the same amount of “pain” signals from our joints can be experienced very differently by different people at different times depending on their psychological and emotional state.
A common example that we see as physiotherapists is a link between a client’s mental health state and their reported levels of pain and functional limitation. Research shows that mental health factors including anxiety, depression, fear of movement, and pain catastrophising are associated with disability and pain flares in people with OA (Wise et al 2009).
All this discussion highlights the old medical saying of “Treat the person not their scan!”. As physio’s and exercise physiologists we design treatment programs based on our client’s history, their goals, main functional limitations, and their physical exam findings in the clinic. We take note of imaging findings if clients have already had scans, however they do not usually play a significant role in planning our initial treatment programs.
MYTH 3: I Should Stop Exercising If I Have Osteoarthritis
 In fact, the reverse is true. Exercise therapy is recommended by ALL guidelines as a first line intervention for OA. Targeted strengthening using a program tailored to your specific situation is one of the most important parts of effective management of hip and knee OA.
In fact, the reverse is true. Exercise therapy is recommended by ALL guidelines as a first line intervention for OA. Targeted strengthening using a program tailored to your specific situation is one of the most important parts of effective management of hip and knee OA.
It’s easy to see why many people believe that exercise will harm the joint cartilage and “wear the joint our faster”. It seems like common sense – more loading will produce more wear and tear and make things worse. But we need to remember the benefits of strength and appropriate levels of loading on our bodies. Research has repeatedly shown that the stronger you are, the less OA-related pain you feel and the better function you have. So, the stronger you are the better you are! This is due to improved joint support and movement control by maintaining strength, and may also relate to better maintenance of cartilage structure through appropriate joint loading.
As well as the physical benefits of exercise for OA, exercise may also help OA management through benefits to our mental health. As noted above, our mood and mental outlook have a big impact on pain perception, and exercise has been extensively proven to improve our mental health, lift our mood, promote a positive mental outlook and combat anxiety and depression.
Exercise should form a foundation for managing OA in most people, but not all exercise is going to be great for every person. The optimal type and intensity of exercise varies from person to person, so being assessed and getting on the right program for you is important. Your physio, exercise physiologist, or appropriately qualified trainer can help you with this.
It’s also worth remembering that exercise is essential in preventing a huge range of other chronic diseases, many of which are common in people with osteoarthritis. If people significantly reduce their levels of physical activity due to OA pain then they are much more at risk of developing conditions including diabetes, cardiovascular disease, excessive weight gain/obesity, and mental health issues. So getting on the right exercise plan is essential for preventing these secondary complications, as well as for directly managing OA.
MYTH 4: There’s Nothing I Can Do To Prevent Or Minimise Osteoarthritis
 Another common belief goes along the lines of “Well, I’m getting older so I’ve just got to expect to be feeling some arthritis pain”. But strong evidence shows that OA can be prevented or reduced by working on some key things known as modifiable risk factors.
Another common belief goes along the lines of “Well, I’m getting older so I’ve just got to expect to be feeling some arthritis pain”. But strong evidence shows that OA can be prevented or reduced by working on some key things known as modifiable risk factors.
One of the biggest risk factors for developing OA in a joint is a previous significant injury to the joint, usually during sport or exercise. Whilst there is always a risk of these injuries when playing sport, you can significantly reduce your risk by completing programs such as the FIFA 11+ or the Netball Australia Knee Program. These have been shown to reduce your risk of knee injury by around 67%, which not only saves you pain in the short term but also reduces your risk of OA in the future.
Being obese (BMI >30) is also a well-established modifiable risk factor, increasing your risk of developing OA in two ways;
- Mechanical Loading: excess body weight means increased mechanical loading of joint structures
- Systemically: obesity changes some metabolic factors that increase your risk of developing OA by inducing pro-inflammatory processes in cartilage and bone
Excessive occupational load (eg sustained kneeling or lifting), leading a very sedentary lifestyle, and muscle weakness have also all been linked to the development of OA. Being active is essential for joint health because it stimulates cartilage regeneration and can promote muscle strength for effective movement control. For these reasons participating in the appropriate types of exercise, strengthening and physical activity are effective ways to reduce your risk of developing OA, and also for minimising symptoms if OA exists.
MYTH 5: Surgery Is The Best Way To Fix Arthritis
 As we have already discussed, research shows that focusing on conservative (i.e. non-surgical) ways to prevent and manage OA brings effective relief to many people. By maintaining the right type and frequency of exercise and activity, building strength, keeping a healthy body weight and preventing joint injuries when possible, many people never need to contemplate surgical options.
As we have already discussed, research shows that focusing on conservative (i.e. non-surgical) ways to prevent and manage OA brings effective relief to many people. By maintaining the right type and frequency of exercise and activity, building strength, keeping a healthy body weight and preventing joint injuries when possible, many people never need to contemplate surgical options.
Current research shows that arthroscopic (keyhole) knee surgery is not better than exercise or cortisone injections for people with symptoms of mild to moderate OA. Therefore a solid program of conservative management should always be the first option for OA management, and surgical intervention should only be considered if conservative measures don’t provide acceptable pain relief.
This doesn’t mean that surgery has no role to play in OA management, only that it should be a last resort and reserved for more severe cases, after conservative options have been fully tried. Total joint replacement surgery can provide effective relief in severe cases of OA, but using conservative management to delay this surgical intervention is very helpful in two ways;
1. replacement joints only have a limited lifespan, so delaying joint replacement surgery can avoid the need for the joint to be replaced a second time
2. maximising your pre-op strength and level of function, plus achieving a healthy body weight, means that your post-op recovery is often faster and brings better long-term results. This is the principle behind “pre-hab” programs. When it comes to surgery, the better you go in the better you come out.
Reference & Acknowledgement
This post is based on an article in the Australian Physiotherapy Association InMotion magazine, May 2021.
Full references available on request.

